Unlock Michigan Medicaid: 5 Key Phone Numbers You Need Now!
Navigating health coverage can often feel like trying to find your way through a maze. For many residents, Michigan Medicaid and the Healthy Michigan Plan are essential lifelines, providing access to vital healthcare services. But knowing who to call when you have a question, need to apply, or want to manage your benefits can be a challenge.
That's where this guide comes in. We've cut through the confusion to give you a direct roadmap to the most important contacts within the Michigan Department of Health and Human Services (MDHHS) system. Forget endless searching and frustrating dead ends. We’re here to connect you with the right person, the first time.
Ready to take control of your healthcare journey? In this article, we’ll break down the 5 key contact points you need to know—from handling your initial Medicaid Application and eligibility questions to accessing your benefits with confidence.
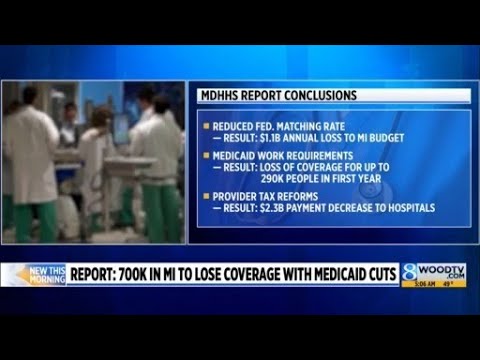
Image taken from the YouTube channel WOOD TV8 , from the video titled Report: 700K in Michigan could lose coverage with Medicaid cuts .
When it comes to essential health coverage, knowing who to contact can make all the difference.
The Direct Route: Connecting with Michigan Medicaid and the Healthy Michigan Plan
For many residents across Michigan, access to affordable and comprehensive healthcare isn't just a convenience—it's a fundamental necessity. In our state, two pivotal programs stand at the forefront of this effort: Michigan Medicaid and the Healthy Michigan Plan. Both are designed to provide vital health coverage, ensuring that individuals and families, particularly those with lower incomes, disabilities, or specific health needs, can receive the medical care they require without overwhelming financial burdens. These programs cover a wide array of services, from routine doctor visits and prescription medications to hospital stays and specialized treatments, acting as a crucial safety net for countless Michiganders.
Navigating a Complex System with Ease
While the benefits of these programs are clear, the administrative structure behind them can often feel like a complex labyrinth. Attempting to pinpoint the exact department or individual who can answer your specific question about eligibility, application status, or benefit access can be frustrating and time-consuming. That's why this guide is designed to cut through the confusion. Our goal is straightforward: to provide you with direct access to the right phone numbers, ensuring you can connect with the appropriate support quickly and efficiently.
The Heart of the System: MDHHS
At the core of Michigan's public health and human services programs is the Michigan Department of Health and Human Services (MDHHS). This state agency is the primary administrative body responsible for overseeing and managing both Michigan Medicaid and the Healthy Michigan Plan. From setting policies and processing applications to managing benefits and addressing inquiries, the MDHHS is the central hub for all program-related operations. Understanding their role is key to understanding where to direct your questions.
Your Essential Contact Points Simplified
To help you seamlessly navigate this system, we've identified five key contact points that cover the most common needs and inquiries. Whether you're just beginning your journey to apply for coverage, have pressing questions about your eligibility, or need assistance accessing your hard-earned benefits, this comprehensive guide will simplify the process. By providing direct lines to the appropriate MDHHS resources, we aim to empower you with the information you need to make the right call, every time.
Now, let's explore the first and most critical point of contact for general inquiries and foundational support.
As you begin to navigate the various resources available for Michigan Medicaid beneficiaries, knowing where to direct your initial inquiries is crucial.
Your Direct Line to Clarity: The Beneficiary Help Line
When you're an enrolled member of Michigan Medicaid and have general questions, the Beneficiary Help Line serves as your primary point of contact. This dedicated resource is designed to be your first stop for a wide range of inquiries, ensuring you get accurate and helpful information directly from the source.
This essential line can assist with several common issues and concerns you might encounter as a Medicaid recipient. They are equipped to help you:
- Understand Covered Services: Get clear explanations about what medical services, prescriptions, and other benefits are covered under your Michigan Medicaid plan. This can help you make informed decisions about your healthcare needs.
- Resolve mihealth Card Problems: If you're experiencing issues with your mihealth Card – perhaps it's lost, stolen, damaged, or not working as expected – the Beneficiary Help Line can guide you through the process of resolving these problems, including how to request a replacement.
- Clarify Medicaid Eligibility Status: You can inquire about your current Medicaid Eligibility status, ensuring you understand your active coverage periods and any requirements for maintaining your benefits.
The Beneficiary Help Line is particularly valuable if you are new to the system, unsure about which Medicaid Health Plan you are currently assigned to, or simply have basic questions about your benefits. It acts as a helpful guide, ensuring you don't get lost in the details of the broader system.
For your convenience, here are the contact details for the Beneficiary Help Line:
| Phone Number | Hours of Operation |
|---|---|
| 1-800-642-3197 | Monday - Friday, 8 a.m. - 7 p.m. EST |
| TDD/TTY: 1-866-501-5656 |
While the Beneficiary Help Line is excellent for general inquiries, some aspects of your Michigan Medicaid experience require a more specialized approach, especially when it comes to actively choosing and managing your health plan.
While the Beneficiary Help Line is your go-to for general Medicaid questions, sometimes you need to take direct action to manage your health care.
Your Personalized Path to Care: Connecting with Michigan Enrolls
Once your Medicaid application receives approval, the next crucial step in securing your healthcare is to choose a specific health plan. This is where Michigan Enrolls becomes your primary resource. Michigan Enrolls is the official enrollment broker for the state, designed specifically to help you navigate and select from the available Medicaid Health Plans in your area. Think of them as your dedicated guide for choosing and managing your health coverage.
Choosing Your Initial Health Plan
The most common reason to contact Michigan Enrolls is to select your initial Medicaid Health Plan. After you receive notification that your Medicaid application has been approved, calling Michigan Enrolls is the essential next step. They will provide you with information about the different health plans available where you live, helping you understand your options and make an informed decision. Without selecting a plan, you won't be able to access the full range of benefits your Medicaid coverage offers.
Beyond Initial Selection: Ongoing Plan Management
Michigan Enrolls serves more purposes than just your initial plan selection. They are also your resource for managing your health plan throughout the year. You might need to contact them for various reasons, including:
- Changing Your Primary Care Doctor (PCP): If you wish to switch to a different primary care doctor within your current health plan, Michigan Enrolls can assist you with this change. Your PCP is your main doctor who provides most of your care and refers you to specialists when needed.
- Switching Health Plans During Open Enrollment: While you generally pick one health plan, there are specific times, known as "open enrollment periods," when you have the opportunity to switch to a different Medicaid Health Plan if you choose. Michigan Enrolls facilitates these changes.
- Finding Specific Providers: If you have a doctor, hospital, or clinic you prefer, Michigan Enrolls can provide valuable information on which available health plans cover those specific providers. This is crucial for ensuring continuity of care with providers you trust.
Michigan Enrolls aims to simplify the process of choosing and managing your Medicaid health plan, ensuring you have access to the care that best suits your needs.
Common Reasons to Call Michigan Enrolls
Here’s a quick overview of why you might need to connect with Michigan Enrolls:
| Reason to Call Michigan Enrolls | What Michigan Enrolls Can Help With |
|---|---|
| Initial Health Plan Selection | Choosing your first Medicaid Health Plan after your application is approved. |
| Changing Your Health Plan | Switching to a different Medicaid Health Plan during an open enrollment period. |
| Finding or Changing Your PCP | Selecting a primary care doctor or changing your current PCP within your plan. |
| Checking Provider Coverage | Determining which plans cover specific doctors, hospitals, or clinics you prefer. |
| Understanding Plan Options | Getting information about the different health plans available in your area. |
By contacting Michigan Enrolls, you take an active role in shaping your healthcare experience. But what if you're still in the process of applying, or need help with other case-specific details?
While Michigan Enrolls serves as an excellent digital hub for exploring health plans, some aspects of your Medicaid journey require direct, hands-on support.
Your Personal Guide: Direct Support for Medicaid at Your Local MDHHS Office
For crucial steps in managing your Medicaid benefits, your Local MDHHS County Office plays an indispensable role, providing the in-person assistance and case management support you need. This office is your primary point of contact for all application and ongoing case management requirements related to your Medicaid benefits, offering tailored help directly from a caseworker.
Core Functions of Your Local MDHHS Office
Your Local MDHHS County Office is equipped to handle several vital aspects of your Medicaid journey, ensuring you have the support necessary to access and maintain your benefits:
- Submitting a New Medicaid Application: If you're applying for Medicaid for the first time, or if you prefer in-person assistance with the application process, your local office is the ideal place to go. Caseworkers can guide you through the necessary forms, answer your questions, and help ensure all required documentation is included.
- Checking Application Status: After submitting your application, you can contact or visit your local office to inquire about its status. This provides a direct line to updates regarding your case and expected processing times.
- Completing Your Annual Medicaid Redetermination: Medicaid eligibility needs to be reviewed annually to confirm continued qualification. Your local office is essential for this redetermination process, helping you submit updated information about your household and income to maintain your benefits without interruption.
Reporting Changes That Affect Your Eligibility
Life circumstances can change, and these changes can impact your Medicaid eligibility. It's crucial to report them promptly to avoid any disruption to your benefits. Your Local MDHHS County Office is the best contact for reporting any significant changes, such as:
- Changes in Income: Whether your income increases or decreases due to a new job, promotion, or reduced hours.
- Adjustments in Household Size: If someone moves into or out of your home, or if there's a birth or death in your family.
- Updates to Your Address: Ensuring your contact information is current so you receive all important communications regarding your Medicaid benefits.
Reporting these changes promptly helps ensure you continue to receive the correct level of support and can prevent issues with your coverage.
MI Bridges vs. In-Person Support
While the MI Bridges online portal is a powerful and recommended tool for self-service—allowing you to apply, check status, and report changes digitally from your own device—the local MDHHS county office offers a unique and invaluable advantage: direct, in-person support from a caseworker. For those who prefer face-to-face interaction, have complex questions that require detailed discussion, or need help navigating the digital tools, the local office provides a vital resource. It ensures that personalized, hands-on guidance is available when you need it most.
Once your Medicaid coverage is established, you may find yourself needing support for specific services, and that's where specialized support lines come in.
While your local MDHHS office is a great resource for general application and case management, some specific, high-value services are best accessed through dedicated channels.
Your Roadmap to Specialized Care: Navigating NEMT and MIHP
Beyond your standard medical appointments, Medicaid offers crucial specialized support for specific needs. These services, often high in value, are typically managed through dedicated programs with their own access points, ensuring you receive timely and appropriate assistance. The two key programs we'll explore here are Non-Emergency Medical Transportation (NEMT) and the Maternal Infant Health Program (MIHP).
Non-Emergency Medical Transportation (NEMT)
For many Medicaid beneficiaries, getting to and from medical appointments can be a significant hurdle. That's where Non-Emergency Medical Transportation (NEMT) steps in.
What is NEMT?
NEMT is a vital service designed to provide rides for Medicaid beneficiaries to scheduled medical, dental, mental health, and substance use disorder appointments when they have no other means of transportation. This can include anything from routine doctor visits to specialist consultations or therapy sessions.
Who Qualifies for NEMT?
If you are a Medicaid beneficiary and lack access to personal transportation, public transit, or rides from family/friends, you generally qualify for NEMT services. The goal is to remove transportation barriers so you can access the healthcare you need.
How to Schedule NEMT Rides
Scheduling a ride is typically straightforward, but it's crucial to know where to start:
- Your Medicaid Health Plan First: For most individuals enrolled in a Medicaid Health Plan (Managed Care Organization), your first call should always be to your specific plan. They coordinate NEMT services directly through their network of transportation providers or a contracted broker. The phone number for NEMT will usually be on the back of your health plan ID card.
- Statewide Contact for Fee-for-Service: If you are not enrolled in a managed care plan (i.e., you are on "Fee-for-Service" Medicaid) or if your health plan directs you, you may need to contact a statewide NEMT coordination line. The contact details for such state-contracted brokers are typically available on the Michigan Department of Health and Human Services (MDHHS) website or by calling the general MDHHS helpline.
Maternal Infant Health Program (MIHP)
The journey through pregnancy and early parenthood is a critical time for both mothers and infants. The Maternal Infant Health Program (MIHP) provides essential support during this period.
What is MIHP?
MIHP is a home visiting service available to pregnant women and infants (up to age one) who are enrolled in Michigan Medicaid. It provides comprehensive support, education, and coordination of care right in your home or a convenient community setting. MIHP staff, often including registered nurses and social workers, help with:
- Healthy Pregnancy: Guidance on nutrition, exercise, stress reduction, and signs of complications.
- Child Development: Support for infant feeding, safe sleep practices, and monitoring developmental milestones.
- Connecting to Resources: Help accessing community resources like WIC, parenting classes, and mental health services.
- Care Coordination: Ensuring you connect with appropriate medical providers and follow recommended care plans.
How to Find an MIHP Provider and Get Connected
Accessing MIHP services is similar to NEMT, with your health plan being the primary gateway:
- Your Medicaid Health Plan: Your specific Medicaid Health Plan is the best resource for finding an MIHP provider in your area. They can help you enroll and connect with a local agency that offers the program.
- MDHHS Website: You can also search for MIHP providers directly on the Michigan Department of Health and Human Services (MDHHS) website, which often has a searchable database or directory.
Key Takeaway: Call Your Health Plan First!
It's important to reiterate that for both NEMT and MIHP, if you are enrolled in a Medicaid Health Plan, your first call should almost always be to your specific health plan. They are designed to coordinate these valuable services directly and can streamline the process of getting you the help you need. Their customer service lines can guide you to the correct internal department or external partner for these specialized programs.
Specialized Support at a Glance
| Service Name | Primary Purpose | How to Access |
|---|---|---|
| Non-Emergency Medical Transportation (NEMT) | Provides rides to scheduled medical, dental, mental health, and substance use disorder appointments for Medicaid beneficiaries who have no other means of transportation. | Call Your Medicaid Health Plan First. They coordinate this service. If not in a plan (Fee-for-Service Medicaid) or directed by your plan, check the MDHHS website for statewide NEMT coordination details. |
| Maternal Infant Health Program (MIHP) | A home visiting service for pregnant women and infants (up to age one) on Medicaid, offering comprehensive support, education, and coordination of care for healthy pregnancies and infant development. | Call Your Medicaid Health Plan First. They can connect you to local MIHP providers. You can also search for providers directly on the Michigan Department of Health and Human Services (MDHHS) website. |
Understanding these specialized services is key to utilizing your Medicaid benefits fully, and knowing who to contact is equally important should you ever need to challenge a decision about your coverage or services.
While Michigan Medicaid offers specialized support lines for specific needs like non-emergency medical transportation or comprehensive health support during pregnancy, you might encounter situations where your core benefits are at risk.
Don't Accept 'No': How to Fight for Your Michigan Medicaid Coverage
Receiving a notice that your Michigan Medicaid benefits are being denied, reduced, or stopped can be a confusing and stressful experience. It’s important to know that you have legal rights and a clear path to challenge such decisions.
When Your Benefits Are Challenged
If you receive an official notice from the Michigan Department of Health and Human Services (MDHHS) informing you that your Medicaid coverage is changing in a way that negatively impacts you – whether it's a denial of a new application, a reduction in existing services, or a complete termination of your benefits – don't panic. This notice is not necessarily the final word. It also typically provides information on how to appeal the decision.
Your Legal Right: The Medicaid Fair Hearing
A Medicaid Fair Hearing is your legal right to appeal a decision made by the MDHHS regarding your Medicaid benefits. Think of it as an opportunity to present your case to an administrative law judge who is independent of the MDHHS division that made the initial decision. This hearing allows you to explain why you believe the decision was incorrect, provide additional information, and argue for the reinstatement or approval of your benefits. It's a crucial part of ensuring due process and fairness within the Medicaid system.
How to Request a Fair Hearing
To formally request a Medicaid Fair Hearing, you must act promptly, as there are strict deadlines, usually within 90 days of the date on your notice. The specific steps and contact information will be provided on the denial, reduction, or termination notice you received from MDHHS. However, the general process involves:
- Review Your Notice: Carefully read the notice. It will explain why your benefits are being changed and the steps to appeal. Pay close attention to any deadlines.
- Contact MDHHS: While the specific number will be on your notice, you can generally reach the Michigan Department of Health and Human Services (MDHHS) Office of Administrative Hearings and Appeals at 1-855-827-7325 (1-855-8-APPEAL). This number is your direct line to initiating the appeal process.
- Be Prepared: When you call, be ready to provide your name, Medicaid ID number, and the date of the notice you received. You'll also need to briefly explain why you are appealing the decision.
- Follow Instructions: You may be asked to submit a written request in addition to your phone call. Ensure you follow all instructions provided by the MDHHS representative to formally submit your appeal.
- Gather Evidence: Collect any documents or information that supports your case, such as medical records, income statements, or letters from doctors. You will have an opportunity to present this at your hearing.
A Useful Aside: The Provider Help Line
While the Medicaid Fair Hearing is exclusively for beneficiaries, it’s worth noting that a Provider Help Line also exists for healthcare providers. This line is specifically for doctors, hospitals, and other healthcare entities that have issues with Medicaid billing, claims, or policy interpretations. While you, as a beneficiary, won't use this line directly, knowing it exists can be useful. For example, if your doctor is experiencing repeated issues getting paid for a service you received and this is impacting your care, you might suggest they contact the Provider Help Line to resolve their billing issue, which could indirectly benefit you by ensuring your provider remains willing to accept Michigan Medicaid.
Equipped with the understanding of your right to appeal, you are taking an active role in shaping your Michigan Medicaid journey and securing the healthcare you need.
Video: Unlock Michigan Medicaid: 5 Key Phone Numbers You Need Now!
Frequently Asked Questions About Michigan Medicaid Phone Numbers
What is the primary phone number to apply for Michigan Medicaid?
To apply for benefits over the phone, you can call the Michigan Department of Health and Human Services (MDHHS) Application and Information line. The correct medicaid michigan phone number to begin the application process is 1-855-275-6424.
How can I check the status of my Medicaid application?
After you apply, you can check your application status by calling the MDHHS Help Desk at 1-844-464-3447. This medicaid michigan phone number can provide information on your case or direct you to the appropriate local office for an update.
Who do I call if I have questions about my current Medicaid benefits?
For current members with questions about coverage, services, or finding a doctor, the Beneficiary Help Line is your best resource. The medicaid michigan phone number for beneficiary support is 1-800-642-3195. They can clarify your benefits and help resolve issues.
Is there a phone number for reporting Medicaid fraud?
Yes, if you suspect fraud, waste, or abuse in the Medicaid program, you should report it. The Office of Inspector General (OIG) has a specific hotline. Use this medicaid michigan phone number to report your concerns: 1-855-643-7283.
Navigating the Michigan Medicaid system doesn’t have to be overwhelming. By keeping this guide handy, you now have the direct lines you need for every situation. Whether it's the Beneficiary Help Line for general questions, Michigan Enrolls to choose a plan, your Local MDHHS County Office for case-specific support, specialized lines for transport, or the number to request a Fair Hearing, the right help is just a phone call away.
We encourage you to bookmark this page for future reference. Staying proactive is the key to a smooth experience. Remember to use powerful self-service tools like MI Bridges whenever possible and maintain open communication with your caseworker to keep your coverage secure.
You are your own best advocate. With these essential contacts at your fingertips, you are fully equipped to manage your health coverage confidently, ensuring you and your family have the support you need to maintain your health and well-being.
Related Posts:
- Top 7 Reasons to Visit Watermark Brewery in Stevensville, MI
- Lake Missaukee, Michigan: 11 Can't-Miss Activities in 2024
- Is Planet Fitness in Michigan City Worth It? 7 Facts to Know
- Unlock New Buffalo, MI: Your 24-Hour Guide to Perfect Timing!
- Proving a Hostile Workplace in MI: 5 Critical Steps to Take
